Defining “need”: (1) the optics of the eye
The eye is a system of lenses to focus an image of an object on your retina so it can be processed and interpreted by your brain. Part of this system, the crystalline lens, is flexible; it changes shape under the control of the ciliary muscle, providing additional optical power to focus on near objects. This is called “accommodation”. What can go wrong with the refractive (focusing) properties of this system?
When looking at distant objects, the most common problem is myopia (short-sightedness, near-sightedness). The system has too much optical power, typically because the eyeball has grown too long. Since the flexible lens can only add yet more power, the eye cannot – unaided – achieve the reduced power required to focus on distant objects. Squinting can deform the eye into a more round shape and partially improve focus, but it is difficult to keep the facial muscles engaged for a sustained period. So myopes (people who are short-sighted) typically add another lens to the system: an external, concave lens with negative optical power to offset the unwanted positive power. Held in a frame, these lenses make a pair of glasses (spectacles).
The eyeball can grow too short as well as too long, giving a system with too little optical power. This is hyperopia (long-sightedness). Fortunately, the crystalline lens can add power, correcting the overall system and bringing distant objects into focus. However, this means that some of the eye’s limited range of accommodation is used up just to focus in the distance, leaving less capacity to focus on near objects (which requires even greater optical power). Accommodation decreases over a lifetime as the crystalline lens becomes stiffer and less responsive to the action of the ciliary muscle. So while younger people tend to be able to offset hyperopia by accommodating, adults will eventually have too little accommodative power. And at every age, hyperopia reduces the ease of focusing on near objects.
A different kind of problem when looking at distant objects is astigmatism: non-symmetrical deformation of the eye such that perpendicular planes have different optical powers. So, for instance, looking at a cross, the vertical bar might be sharp whilst the horizontal bar is blurred. Adding an appropriate asymmetric external lens to the system can offset the error. So the prescription for a pair of glasses might include an asymmetrical element of “cylinder” and its radial “axis” in addition to the “spherical” element. However, other than in cases of severe astigmatism, clear vision can be achieved with the “best sphere” lens that offers the optimal compromise in the sharpness of perpendicular planes (see our research).
When looking at near objects, the question is whether the eye has enough accommodation – whether the crystalline lens can add enough optical power – to bring the focus near enough. As accommodation decreases over a lifetime, it becomes harder to focus on closer objects. This is presbyopia. Typically, people over 45 years will need reading glasses to provide a boost of positive power. (Myopes wearing glasses for distance correction may simply take them off, leaving the unaided eye with its default near focus.) Eventually, as accommodation continues to decrease, people lose all ability to change their focal distance. At this point, even the boost from reading glasses is not a complete solution because it simply brings the focus to a fixed near distance without providing any of the flexibility to accommodate slightly closer objects. Depth of focus – the range of distances which are all in focus at one time – becomes more important. Lower light levels – requiring a larger pupil and thus reduced depth of focus – can make it difficult to see near objects clearly, even with reading glasses. Some older people use glasses with varifocal lenses, which provide a gradation of increasing power towards the bottom of the lens so that there will be one particular angle at which an object at a given distance is in focus (the downside being that no object is ever in focus across the whole lens, reducing the effective field of vision).
In conclusion, the two most commonly required kinds of refractive correction are:
- negative-power (spherical) lenses for myopia and/or mild astigmatism in children and adults; and
- positive-power lenses for presbyopia in older adults (and for severe hyperopia in children).
The reason for distinguishing these two categories is the different degree of accuracy of lens power required in each case to be able to see clearly. Give presbyopes a choice between +1.5D and +2.5D lenses (the dioptre, D, is a unit of optical power) with the same power lens for left and right eyes and most of them will achieve good near visual acuity (sharpness of vision). That is because they need only an approximate boost of postive power: their residual accommodation allows them to fine tune their focal distance (provided that their corrective lenses err on the side of being too weak rather than too strong; and that they are not so old as to have lost all power of accommodation). In many situations they can also move their head or change the distance at which they hold an object in order to give further control over the sharpness of the image.
In contrast, ask myopes or mild hyperopes to choose between -1.5D, -2.5D and -3.5D lenses (again, same power in left and right lenses) and most of them will end up with poor visual acuity. Hence the distinction in the conventional eye care industry between reading glasses sold over the counter to presbyopic customers, who can try on the different lens powers unsupervised and select which pair of glasses works for them; and on the other hand, for myopic customers, the bespoke assembly of a frame with a pair of lenses made in accordance with a prescription generated by a highly trained eye care professional using specialist equipment.
Where this really starts to matter is in the developing world where eye care professionals are few and (very) far between: compare the ratio of clinical refractionists to population of about 1:10,000 in most developed countries with a ratio closer to 1:1,000,000 in many developing countries. The conventional over-the-counter model for reading glasses can be adapted for poor, rural customers served by minimally trained local entrepreneurs, for instance. In contrast, the conventional approach to serving myopes cannot get off the ground without the professional and logistical infrastructure of the developed world’s eye care industry.
Defining “need”: (2) functional requirements
When did I first need glasses? I was 12 years old when I first looked at an eye chart (see below). It was not part of a formal eye test so nobody else noticed that I had to squint to read the smallest letters. I noticed, though, and afterwards I realised that sometimes I had to squint to read road signs. But I did not have a formal diagnosis or a prescription and I certainly did not wear glasses. At that point I must have had some refractive error, probably more than one dioptre of myopia. Did I need glasses?
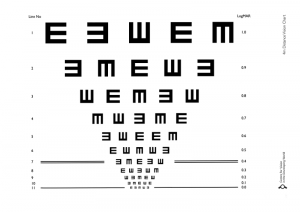
An eye chart with the optotype “E” pointing in different directions, for people who may be illiterate or use a different alphabet and are thus unable easily to identify Latin characters. The optotypes decrease in size in each line; the lowest line from which optotypes can be reliably identified by a person at a given distance from the chart defines that person’s visual acuity.
About six months later, I started at a new school and the nurse carried out a quick visual acuity screening. I could not read the smallest letters and I was told to go for an eye test. My mother took me to an optometrist, who carried out a refraction and gave me my first prescription for myopia: -1.25D in the right eye and -1.5D in the left eye (I was also prescribed 0.5D of cylinder in each eye for astigmatism). I received my first pair of glasses. I had never previously paid much attention when other kids wore glasses but now I felt embarrassed and I wore them only in class and only while I needed to read something on the blackboard – the rest of the time they sat on my desk. Outside class, I wore them only at the cinema. Later I started to play tennis competitively and found I was better able to return serve if I wore my glasses – though I could still play without glasses much of the time. Did I need glasses?
It is conventional to define the need for glasses in terms of a given refractive error (the optical power specified on an optometrist’s prescription) or visual acuity: the smallest letters on an eye chart that I can reliably resolve – often specified as a fraction, e.g. 20/20 (also written as 6/6), the standard to which an optometrist hopes to correct most patients; or 20/40 (6/12), the minimum legal standard to pass a driving test in many countries. But what I will argue here is that a given acuity standard only makes sense within a particular functional context. The fact that there is a driving sight test is a clue. I need a visual acuity of at least 20/40 to drive safely, but with that acuity I would struggle to read the smaller letters on the blackboard from the back of a classroom. So in class, I need an acuity of 20/25, say. The functional context – what I am trying to do – determines how clearly I need to be able to see and therefore whether I need glasses. At any given time, whether I need glasses depends on the nature of my work and leisure activities – am I in school, do I drive a car, do I like to be able to see the facial expression of someone standing across the room from me at a social event? I suggest that there is an essentially subjective aspect to whether a given individual needs glasses, in addition to the objective fact of their refractive error.
In some circumstances, public policy overrides subjective preference: the law requires you to wear glasses to achieve a certain minimum acuity when driving, whatever your subjective preference, in order to protect other road users (on the basis that poor visual acuity increases the risk of a road traffic accident). Similarly, there is, I suggest, a moral imperative to ensure that children in school wear the glasses they need to read everything on the blackboard in order to get the full benefit of their education – even if they hate wearing glasses and would rather not. But beyond these cases, we need to recognise that different functional contexts and subjective preferences will set different thresholds of refractive error or visual acuity beyond which there is a need for glasses (or contact lenses or refractive surgery, in parts of the world where those options are available).
Even the relation between refractive error (e.g. -2 D) and visual acuity (e.g. 20/60) is context-dependent: the illustration below shows how the same refractive error – in this case -2 D, about my degree of myopia today – gives very different visual acuity in different light levels. Below left, with good illumination, the pupil diameter is 3 mm and the image relatively sharp; below right, in poor light, the pupil diameter expands to 8 mm so that enough light reaches the retina to form an image, but the greater effect of aberrations (because the optical system of the eye is not perfect) produces a more blurred image.
It is not just visual acuity that determines how well we can function in a given context. Field of vision is also important. For instance, when driving it can be more important to have good peripheral vision than to be able to see clearly straight ahead. What a pair of glasses needs to be – and whether glasses are needed at all – depends on what the person is trying to do.
In conclusion, when we talk about the need for glasses, we should pay attention to the functional context. It is reasonable to claim that all schoolchildren and all drivers need glasses if they would not otherwise have good visual acuity. What is good enough acuity depends on the task at hand. It may also be reasonable to claim that all presbyopes (older adults who can no longer focus on near objects) need glasses – at least if they want to be able to read or use a phone. But I suggest we should be careful about setting more or less arbitrary criteria for needing glasses in terms of refractive error or visual acuity. Need depends on functional context.